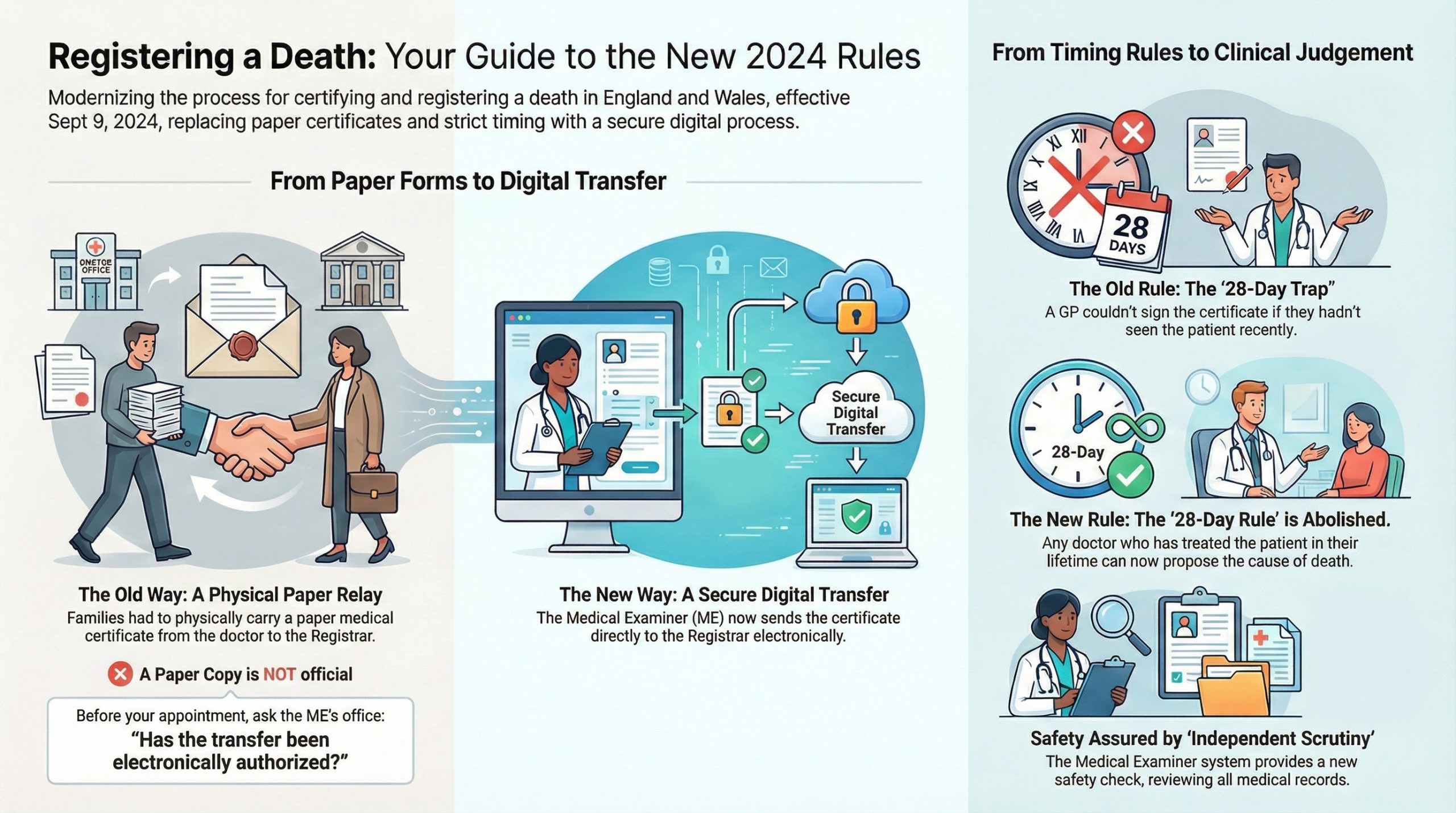
For decades, the “Green Form” and the “Medical Certificate of Cause of Death” (MCCD) were physical talismans. Grieving families would wait at a GP surgery or hospital bereavement office, be handed an envelope, and physically carry that paper to the Register Office. It was a tangible, albeit heavy, part of the process.
As of September 9, 2024, that physical relay has been legally abolished.
If you arrive at a Register Office today holding a paper MCCD given to you by a doctor, you are likely to be turned away. This guide explains the technical logic of the new Electronic Transfer system and how to ensure the “digital baton” has been passed before you leave your house.
1. The “Paper Draft” Trap
One of the most common points of friction in the new system occurs when a doctor or hospital staff member prints out a “copy” of the MCCD for the family. While this is helpful for your records, it has no legal standing at the Register Office.
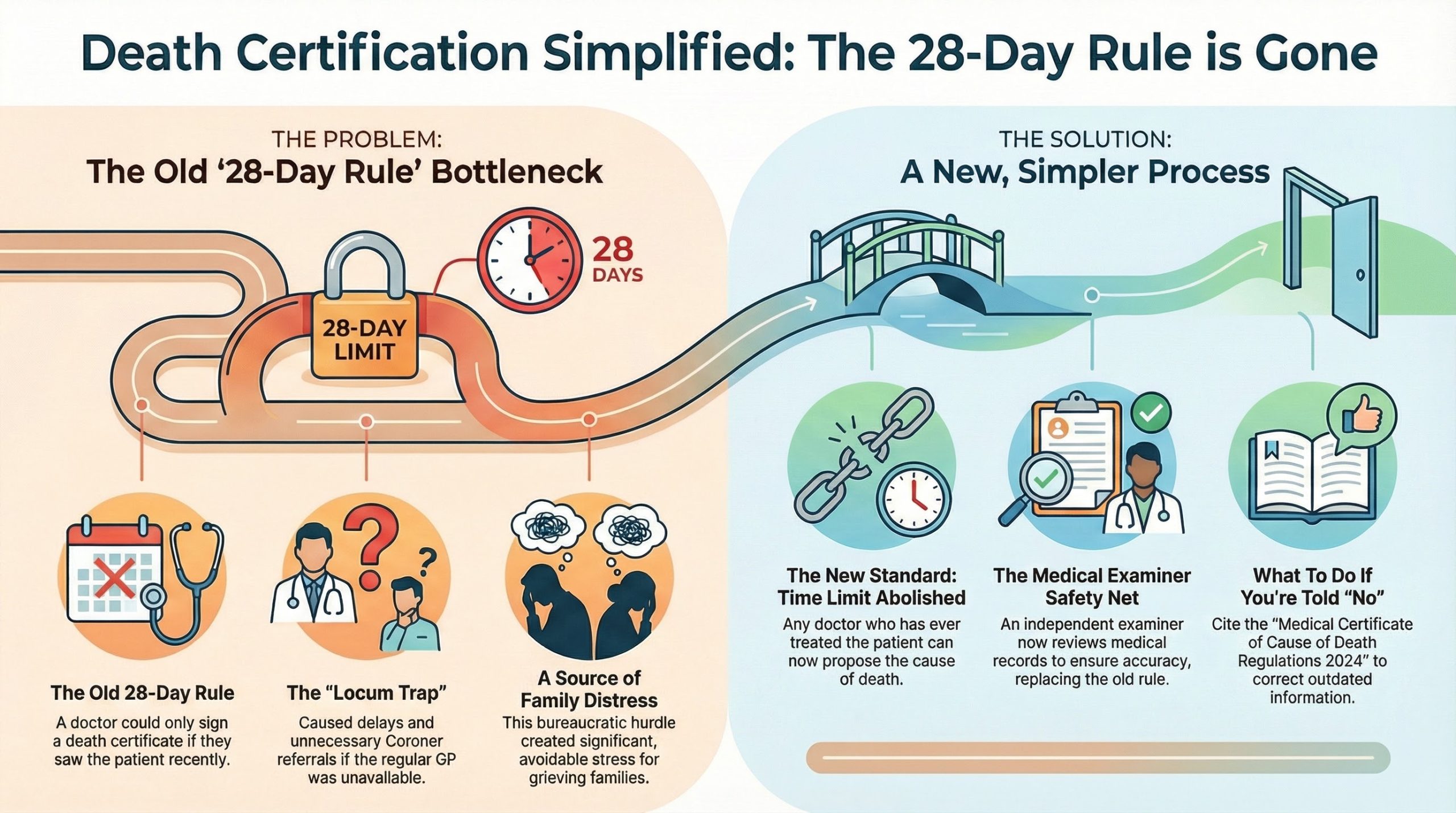
The Technical Reality: Under the Medical Certificate of Cause of Death Regulations 2024, the Registrar is prohibited from registering a death based on a paper document presented by the family. They can only proceed once they receive a secure, encrypted electronic notification directly from the Medical Examiner’s (ME) office.
2. The “Scrutiny Complete” Flag
The reason for this digital-only approach is the mandatory scrutiny phase. In the old system, the GP’s signature was the final word. In the new system, the process looks like this:
- The Doctor drafts the MCCD digitally.
- The Medical Examiner reviews the digital file and performs “Independent Scrutiny.”
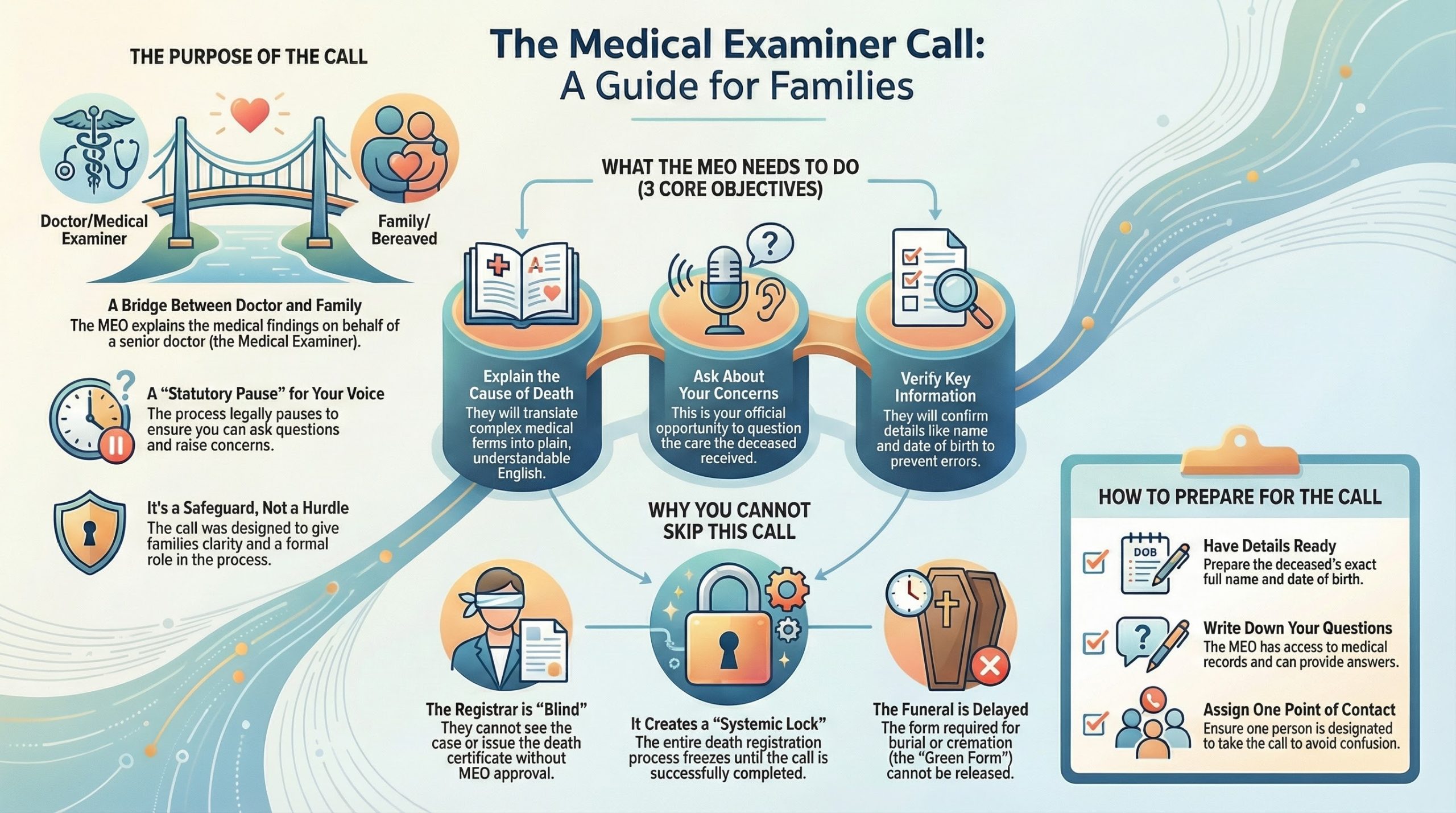
- The Family Discussion takes place via a Medical Examiner Officer (MEO).
- The ME Digital Signature: Once the ME is satisfied, they click “Authorize.” This sends the file through a national portal directly to the Registrar in the district where the death occurred.
If you have the paper but the ME hasn’t clicked “Authorize,” the Registrar literally cannot see the death on their screen. To them, the person hasn’t officially “passed through the system” yet.
3. Why the Registrar Will Turn You Away
Registrars now operate on an appointment-only basis with very tight windows. If you book an appointment and turn up with a paper form, but the digital transfer hasn’t arrived, the Registrar cannot:
- Verify the cause of death.
- Issue the “Green Form” for the funeral.
- Issue the official Death Certificates.
This results in wasted time, increased family distress, and the need to re-book—often days later. This is a failure of “Unreasonable Hospitality” in the public sector, but you can avoid it by knowing the digital status.
4. How to Verify the Digital Transfer
To ensure you aren’t walking into a “Registration Trap,” follow these steps before your appointment:
- Ask the “Authorization” Question: Don’t ask the GP if the form is “ready.” Ask the Medical Examiner Officer: “Has the Medical Examiner electronically authorized the transfer to the Registrar yet?”
- Wait for the Email/SMS: Many Medical Examiner offices now send an automated notification to the family once the electronic transfer is successful.
- The “Register by Declaration” Exception: If you are registering a death in a different city (by declaration), the electronic transfer must still go to the original district first, which then coordinates with your local office. This adds an extra digital layer that requires verification.
5. Frequently Asked Questions (FAQ)
Q: Can I email a scan of the paper MCCD to the Registrar? A: No. The Registrar will only accept the version sent via the secure NHS/General Register Office (GRO) portal.
Q: What if the doctor says they “don’t do” electronic transfers? A: All GP surgeries and hospitals in England and Wales are now required to use this system. If they are refusing, they are in breach of the 2024 regulations.
Q: Does this apply to Coroner cases? A: No. If the Coroner is involved, they use a different form (Form 100) which is also sent electronically to the Registrar, but the workflow bypasses the standard Medical Examiner route.
Expert Summary
The shift to digital is designed to prevent fraud and errors, but it has removed the “tangible” certainty of holding the paperwork. As an Executor, your new “baton” is the confirmation of a digital transfer.
Before you step foot in a Register Office, ensure the digital handshake between the ME and the Registrar has been completed. For further support in coordinating the first family meeting after these hurdles are cleared, you can find resources at the Sunday Roast Forecaster.
Next Step: Once the digital transfer is confirmed, your next hurdle is the registration appointment itself. Use our 72-Hour Limbo Checker to monitor the status of your case in real-time.